1. Introduction
The human eye is an organ that combines singular anatomical and histological characteristics with complex physiological properties to develop its function as an image formation “device”. Among the multiple conditions that can impair vision, the cataract is the most common one, and is the most frequent surgical intervention. The development of artificial intraocular lenses (IOLs) to compensate the removal of the natural crystalline lens after cataract requires a detailed study of the optical properties of the human eye. Also common are refraction and aberration conditions, such as myopia or astigmatism, and optical benches to design and test spectacles or contact lenses (CLs) are also widely required. In addition, with the advance of optical testing devices and techniques for physiological applications, there has also been an increased interest in providing dummy eyes to validate CLs and IOLs. New treatments such as laser interventions have also been tested in vitro.
Compared to other physiological systems, there is a strong interest in physical modeling of the optics of the eye. Due to their small dimensionality and complexity, mere computer theoretical models are usually not practical for assessing quality of vision, designing optical implants or measurement devices, or planning and monitoring treatments. One of the main challenges is to be able to predict the subjective response of a patient prior to actually altering his/her vision, either surgically or by external means such as spectacles or contact lenses. An additional problem is the fact that the eye characteristics present large inter-individual variability, which means that the models need to be highly customizable. Thus, the ability to accurately predict the in vivo performance of constantly changing ocular parameters has many obvious advantages over theoretical computer models, with the goal of reducing the time, cost, and uncertainty involved in efforts to improve visual quality. For these reasons, there has been an increase in the development of physical models of the eye in the last decades, in order to conduct preliminary tests (bench testing) of image formation capabilities of optical devices for physiological applications. This interest was boosted by the increased complexity of the design in recent years.
An optomechanical eye model (OME), sometimes called optomechanical artificial eye model (OMAE), or physical artificial eye model, is a customizable system that tries to mimic the anatomy and function of the human eye in vitro. Various efforts had been made to build realistic physical eye models. While initial devices were based mainly on the well-known Gullstrand reduced eye model [1], nowadays, eye models are way more complex, detailed and varied. Eye models are widely used as benchmarks to evaluate the performance of spectacles, contact lens (CLs) and intraocular lenses (IOLs), and are also used to test and calibrate optical measurement devices, new surgical interventions and for use in research studies.
Besides the fields of physiological optics, optometry, ophthalmology or biomedical engineering, the global mass production industry has taken advantage of the advances in artificial vision capability to assist in quality control, as well as other parts of the production, storage and delivery processes. This is usually conducted with devices developed for other purposes, which might provide high imaging performance capabilities, but are not intended to reproduce the visual capabilities of the human eye. Additionally, there are tasks that still require the intervention of a human observer to analyze if the products carry defects that could be detected by a human observer. Using the same automatic processes comes with the risk of over-detecting failures that would be never detected by a human observer. Therefore, there is a growing interest to use eye models that can mimic the imaging characteristics of the human eye to replace human observers in tedious processes that require human intervention.
The present review summarizes some of the physical artificial eye models developed in the field of physiological optics to test and mimic the human vision conditions and the effect of artificial devices to compensate vision problems or to test the effects of surgical interventions. Considering that the main applications are in the domain of physiological optics and biomedical engineering connected with applications in the field of visual optics, optometry and ophthalmology, a literature review was conducted using the “PubMed” database as the main source, complemented by searches in different patent databases. Only publications in the English language were considered, despite eye models in other languages having also been found [2]. An additional search was performed for components that may be useful for use in eye models, mainly tunable lenses to mimic the crystalline lens activity or curved sensors to emulate the retinal shape. Although only in vitro physical models are considered, some schematic theoretical models will also be mentioned, when necessary, since they are important references for physical models. Among the artificial eye models reviewed, the main focus is on the subset of devices for human vision applications, while briefly mentioning devices for other applications.
A total of 70 articles and eight patents were found, and are listed in Table 1. If the same eye model is presented in more than one publication involving approximately the same research team, the most relevant one will be preferred, while still mentioning the related publications. After excluding those that were not related to applications in human vision, a total of 13 articles and four patents were selected for a deeper analysis. Nonetheless, the remaining publications will also be considered, but in less detail.
Before discussing the different eye models, the different model types and their main applications are summarized in the next section. Later, a general overview of the basic components included in an artificial model is presented, followed by a debate on how they are assembled. A discussion section includes a general overview of the performance, advantages and disadvantages of the different devices presented, as well as some guidelines, suggestions, and personal comments about physical eye models.
2. Physical Eye Models and Their Applications
Based on theoretical simulations, Gliddon (1929) [3] showed that it was possible to build an optical replica of the human eye for the study of the retinal image. The replica consisted of a copper cell which could be filled with fluid, included a movable mount with a glass retina, replaceable diaphragms to mimic the iris and pupil, double-shell glass lenses with water in between, to model the cornea and crystalline lens, that were placed in magnetic holders that could be moved so that the cornea or lens, or both, could be tipped and decentered. The model was tested on a bench, and the image at the retinal glass was examined with the help of an objective and an eyepiece. This eye model was very detailed for the time it was constructed, and included many of the foundations of modern eye models.
Other eye models followed. In 1978, Arell and Kolari [4] constructed a low-cost adjustable artificial eye model with approximately the real focal length, to use as an object in direct and indirect ophthalmoscopy, as a laboratory experiment for medical and biology students.
In 1987, Heath and collaborators [5] wanted to map distortions associated with ophthalmic lenses. They created a device that consisted of a pinhole camera and a lens holder, where an ophthalmic lens could be placed. The lens mount was designed to include various pantoscopic tilt positions and also allowed for horizontal and vertical rotation around a point to simulate the lens/eye relation when the eye position is changed. The pinhole camera represented the human eye, while its thin film could be viewed as the retina. Despite not being sophisticated and requiring prolonged light exposure, this simple device was one of the first eye model precursors to make it possible to capture and record a retinal image.
In 1992, Rudnicka et al. [6] constructed a physical eye model based on the Bennett and Rabbetts schematic eye [81]. It incorporated a cornea, a lens, and a spherical fundus. The vitreous chamber depth could be precisely varied to produce axial ametropia from −11D to −17D [6]. The optical performance of the model eye was tested with a refractometer, and then the device was used to investigate the relationship between the actual size of a fundus feature and its photographic image in two different fundus cameras.
Still in 1992, Portney [82] presented a method for in vitro IOL inspection, by showing theoretically that a wet eye cell can be designed to be optically equivalent to theoretical eye models. The cell model used was a combination of a wet-cell with a conjugation lens to act as the cornea. A wet-cell is typically a transparent glass cuvette filled with water, where an IOL is immersed for analysis. The use of water cells to evaluate IOLs had been previously described by Holladay [8,9], and is currently a widely popular technique for this application, existing several in vitro eye models based on them.
Today, the International Organization for Standardization (ISO) 11979-2 [83] for evaluation of imaging quality of IOLs provides a model eye with an essentially aberration-free artificial cornea. It consists of a wet-cell with two parallel glass plates made of BK7 glass, which are filled with saline solution with refraction index of 1.336 (546.1 nm) at 35 °C (optional heating) [84]. Several artificial eye models are based on this standard, and some will be mentioned later in this review. A more recent version of the same ISO standard introduced an alternative cornea with spherical aberration, to better mimic the human eye [85].
Artificial eye models have been used for various types of applications. The most common is to evaluate lenses, mainly IOLs, but also CLs or spectacles. Eye models are also widely used for the validation and calibration of ophthalmic equipment. Another type of applications is the evaluation of measurement methods applied to ophthalmology, and the in vitro testing of new surgical treatments.
Another great interest of using physical eye models is to simulate/model selected optical characteristics of the natural eye, for research applications. For example, there have been reported applications to simulate eye measurements in a controlled in vitro environment, to model function such as accommodation, and to simulate human vision under various optical conditions, such as when driving at night, reading text, or recognizing objects. Finally, eye models have also been used for teaching and education purposes, and for potential use in optical design. Table 2 summarizes the main applications of each device presented in this review. This does not mean that the devices are not fit for other uses, but only that these are their intended applications as reported in the publications reviewed.
Eye models for non-optical applications, such as dummy eye models for surgical training, to evaluate eye tracking devices, to validate ultrasound measurements, or to simulate eye movements, will not be considered in this review (see, for example, refs. [86,87,88,89,90]).
3. Measurement Modalities of Eye Models
Considering only the physical eye models for optical-related applications, they can be divided into six main measurement modalities: wavefront measurements; single-pass measurements; double-pass measurements; Scheimpflug or Purkinje imaging; fundus imaging and retinoscopy; and biometry and optical coherence tomography (OCT) measurements. Other non-optical modalities, such as ultrasound measurements (Ref. [52] reported ultrasound biomicroscopy for device characterization, and a dummy eye model for ultrasound biometry is commercially available at [90]), thermal measurements [70], or mechanical and structural characterizations [55], will not be considered in this review, unless the model itself presents relevant features related to optical measurements. Table 3 organizes the main modalities of the respective devices mentioned in this review. Some devices are “multi-modal”, and more than one measurement modality was reported in the respective publications [28,35,37,41,42,48,52,55,64,70,72,80].
This review is focused on the devices used for single-pass complex scene imaging, which are the ones most associated with human vision applications. The next sub-sections briefly discuss the optical modalities and respective eye models existent in literature. The following section focuses on human vision.
3.1. Double-Pass Measurements
The double-pass (DP) technique is a half-century-old method based in the recording of the retinal image after passing twice through the ocular media, i.e., before and after retinal reflection. This method provides accurate estimates of the eye’s image quality, in the form of metrics such as the modulation transfer function (MTF) or the optical transfer function (OTF), which gives information on the overall optical performance of the eye, including all the optical defects involved in retinal image degradation, such as diffraction, aberrations, and scattering [91]. This method is particularly powerful in evaluating many of the conditions that especially affect scattering, but is now less popular for wavefront measurements.
While most eye measurements involve the light to pass twice through the eye, in a double-pass experiment, both passes provide information about the eye optics. Measurements such as fundus imaging only use information from the second pass, and some wavefront measurements are double-pass, while others are second-pass (such as HS aberrometry). This section includes only methods that rely on both passes and do not involve wavefront measurements (discussed in the next sub-section), focusing instead on measures such as the MTF. In addition, only when light is reflected by the retina surface is it considered a double-pass. Scheimpflug and Purkinje reflections are therefore not considered as such.
Eye models for double-pass measurements are characterized by the use of a camera sensor which is located usually outside and in front of the eye (mirrors are used when that is not possible), in order to capture a retinal image that was reflected back to outside the eye. As in wavefront measurements, the retina is also commonly a diffuse reflector. The model previously described by Rudnicka et al. [6] was characterized using autorefractometry, despite this was not its main purpose. The eye model described by Pujol et al. [8] consisted of a simple setup using an achromatic lens as the cornea and a diffuser which could rotate in order to avoid the influence of speckle. Additional lenses with no spherical power and different cylindrical powers were applied to evaluate astigmatism based on cross-cylinder examination methods. The model of García-Guerra [59] previously mentioned double-pass techniques that are also used. The patent by Niven [79] described an eye model for development purposes, with an orange acrylic endcap for use with double-pass measurements. Another simple model was built by Goncharov et al. [35] to measure wavefront aberrations through double-pass experiments using an interferometer, whose data would be used to fit theoretical eye models, in an inverse optical design approach.
3.2. Wavefront Measurements
Wavefront measurements have gained increasing popularity in the last two decades for measuring ocular optical aberrations, as they can objectively characterize the properties of optical systems, including the human eye that is physiological aberrated by the shape of the refractive surfaces. Such aberrations affect the image quality and the visual performance. Additionally, several corrective and surgical interventions further modify the aberration wavefront properties of the eye. Probably the most well-known wavefront sensor is the Hartmann-Shack (HS) sensor, present in most clinical aberrometers. The main drawback of wavefront sensors is the lack of information on scattering [91].
Being an increasingly popular technique, it is expected that there are quite a few artificial eye models related with wavefront measurements. The main characteristic of these models is the retinal surface, which is usually a diffuser that can often rotate in order to avoid speckle noise and destroy the spatial coherence of input light. The light source is typically a laser, while the measurement equipment is typically the Hartmann-Shack (HS) sensor. The analysis often consists in the wavefront reconstruction quantitative characterization of aberrations, and evaluation of metrics such as Zernike or Seidel coefficients.
Eye models have been used together with wavefront measurements in order to validate wavefront measuring devices [15,78], for adaptative optics testing using HS sensors [24], or to evaluate ophthalmic lens [32,41,44,77]. These models are usually designed in such a way it is easy to add and control aberrations. For example, Yamaguchi et al. [78] used a phase plate for that purpose, while [24] used a tunable crystalline lens, and Letfullin et al. [17] and Galetskiĭ et al. [21] used biomorph mirrors to reproduce aberrations and their temporal dynamics in real time. More minimalistic models have also been used, such as by Shen et al. [34] or Guerra et al. [59]. The latter used a combination of data obtained from double-pass and HS measurements to perform estimations of aberrations and scattering in the human eye. The complete model of Bakaraju et al. [37] also allowed a mode for wavefront measurements using a COAS aberrometer, and will be described in a later section. Norrby et al. [23] also presented wavefront measurements using his device. Esteve-Taboada et al. [57] and Drauschke et al. [48] also used wavefront measurements, but only to characterize the eye model aberrations. Moreno-Barriuso et al. [9] used a set of models where HS wavefront measurements were compared with laser ray-tracing (LRT) methods, in both a single-pass and a double-pass manner.
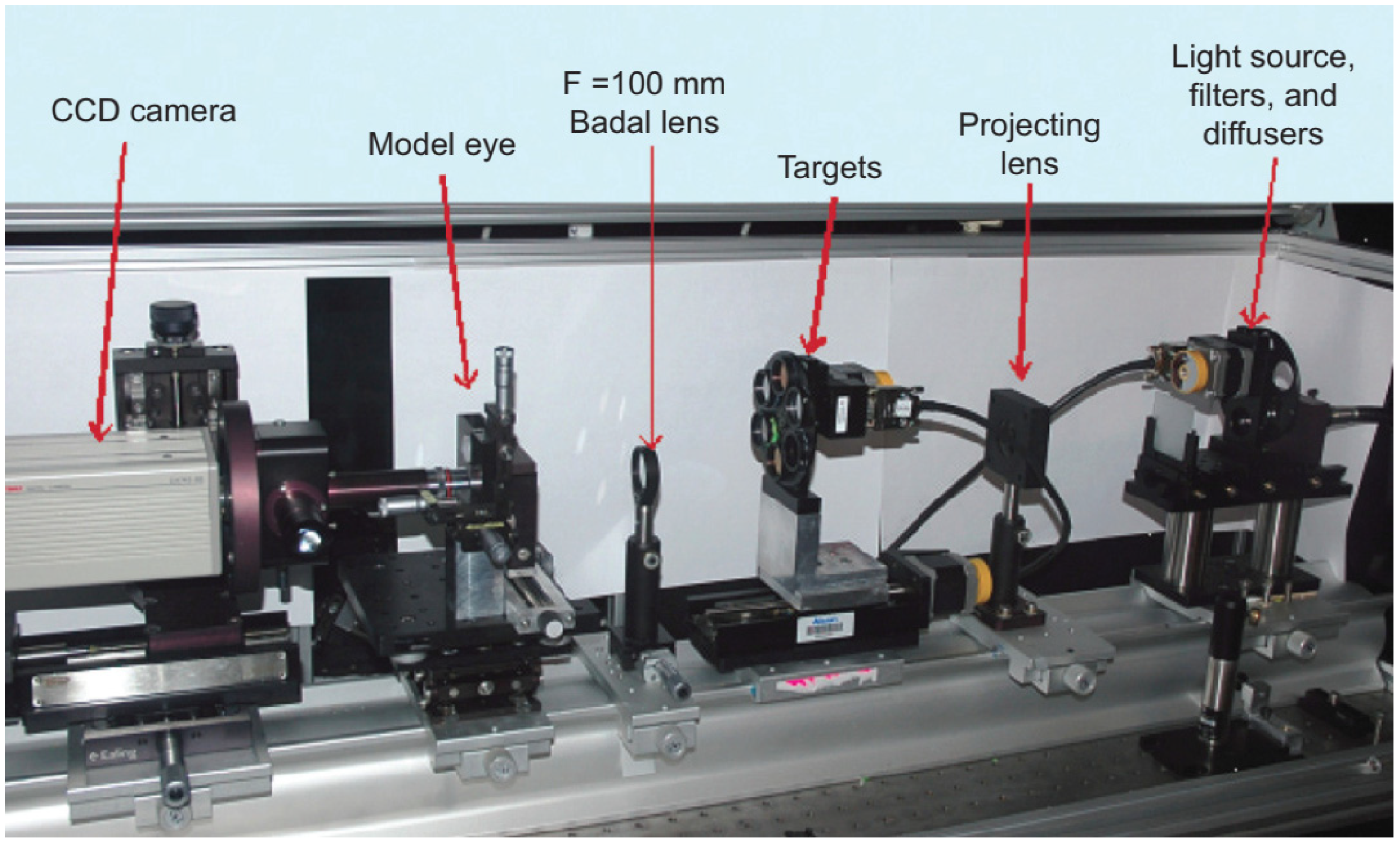
A model that is more detailed was built by Campbell [28]. It was designed to investigate whether wavefront measurements obtained in eyes that have implanted multifocal IOLs gave reliable guidance on creating laser refractive surgical treatments to remove residual refractive error from those eyes. This system allowed for both HS or single-pass measurements, by exchanging a painted surface retina by a glass window connected to a charge-coupled device (CCD) camera through a microscope. However, the latter was used only to set the system for emmetropia with the help of a Badal optometer, by adjusting the length of the eye until the best point spread was observed with the camera system. Then, the transparent window was replaced by the solid retina for the aberration measurements. A schematic representation of this device is in Figure 1.
Wavefront measurements were also performed in reverse direction, using a light source at the level of the retina and the sensor in front of the eye. These measurements are typically called second-pass measurements. Esteve-Taboada et al. [57] designed an opto-mechanical artificial eye for second-pass aberrometer measurements, with the purpose of avoiding the disadvantages of double-pass measurements. A near infrared (NIR) light emitting diode (LED) was used together with a diffuser, to function as an active retina. A diaphragm centered with respect to the rest of the device’s optical components made it possible to limit the amount of light emitted by the retina. The device also had accommodative ability through the use of a lens with an electronically variable focal length, to control the refractive state of the device. A second diaphragm iris (artificial pupil) was added just after the variable lens to acts as the aperture diaphragm of the system (Figure 2). If desired, a wet-cell with an IOL could be placed inside, near the artificial pupil. A commercial HS aberrometer was used to characterize the aberrations of the system.
Coughlan et al. [64] presented an opto-mechanical artificial eye that could be used for examining multi-wavelength ophthalmic instruments. The model was based on the schematic eye of Escudero-Sanz and Navarro [92]. The retina was modeled with a semi-transparent disc and field-stop, and its design offered two modes of operation: HS aberrometry to measure longitudinal chromatic aberration and the possibility of inducing refractive error, for on-axis testing; and second-pass measurements, by back-illuminating the retinal surface and using a CMOS detector, to investigate off-axis chromatic aberration. Due to the ability of performing second-pass measurements on the eye model, the authors said it had a “dispersive design”. The invention described by Altmann et al. [77] also mentions back-illumination.
3.3. Single-Pass Measurements
Single-pass measurements would be the most desired modality for most applications, as they are simpler and have less limitations compared to double-pass measurements, because there is not the problem of specular reflections occurring in the different refractive surfaces. Unfortunately, these measurements are not realistic, as they require measuring light at the retinal surface, which is not possible in vivo with human eyes. The only single-pass measurement we can do in vivo today is still our own natural retinal processing. Therefore, eye models offer a great tool for this purpose, as we can freely implement a CCD camera or other sensor in the artificial eye. For this reason, it is not surprising that eye models aimed at single-pass models are the ones most commonly reported in literature (Table 2).
The most common performance metric to be measured using the single-pass technique is the modulation transfer function (MTF), which is determined by using the magnitude of the Fourier domain analysis. It reveals how different spatial frequencies are handled by the optical system, and can be measured directly via a cross-target or point-/spot-target to obtain the line or the point spread function (LSF, PSF) resulting from imaging a thin line or point of light, respectively [84]. This can be done using trans-illuminated frequency charts (MTF tests), such as the ones referred to by the ISO standards [83], or punctual light sources, such light-emitting-diodes (LED) or lasers, often collimated and filtered. More comprehensive analysis is obtained distinguishing between the sagittal and tangential MTFs, using targets with different orientations [57]. Other types of test include the 1951 United States Air Force (USAF) and Snellen charts, while other cases have used the Sloan letters instead [41].
One of the earliest physical models for single-pass measurements was used by Oshika and Shiokawa [1], in order to assess the effect of soft acrylic IOLs folding procedures on MTF and resolving power [7]. The model eye was based on Gullstrand’s exact schematic eye. The MTF and resolving power were measured under veiling glare light.
The vast majority of single-pass eye models have been used in bench measurements to evaluate IOLs, using the 1999 ISO specifications described before [83]. They can follow this standard strictly [14,18,19,25,29,43,47,49,60,65], or implement slight modifications, namely by using modified corneas to better represent the human cornea or simulate various aberration conditions [13,27,29,31,33,43,50,56,68,71]. Indeed, the most recent iteration of the ISO standard (2014) introduced a new cornea with similar modifications [85]. Figure 3 presents a typical optical bench setup using a wet-cell model to evaluate IOLs ([50]). A microscope is often used to magnify the image at a transparent retinal surface and forward it to a CCD used to produce the retinal images. Figure 4 presents a typical schematic representation of such a configuration ([25]).
Figure 3.
Typical setup of the ISO 11979–2 optical bench setup to evaluate the optical quality of IOLs, using a wet-cell eye model, and a Badal optometer (optional). Clinical Ophthalmology 2014:8 2105–2113 ([50]). Originally published by and reprinted with permission from Dove Medical Press Ltd.
Figure 3.
Typical setup of the ISO 11979–2 optical bench setup to evaluate the optical quality of IOLs, using a wet-cell eye model, and a Badal optometer (optional). Clinical Ophthalmology 2014:8 2105–2113 ([50]). Originally published by and reprinted with permission from Dove Medical Press Ltd.
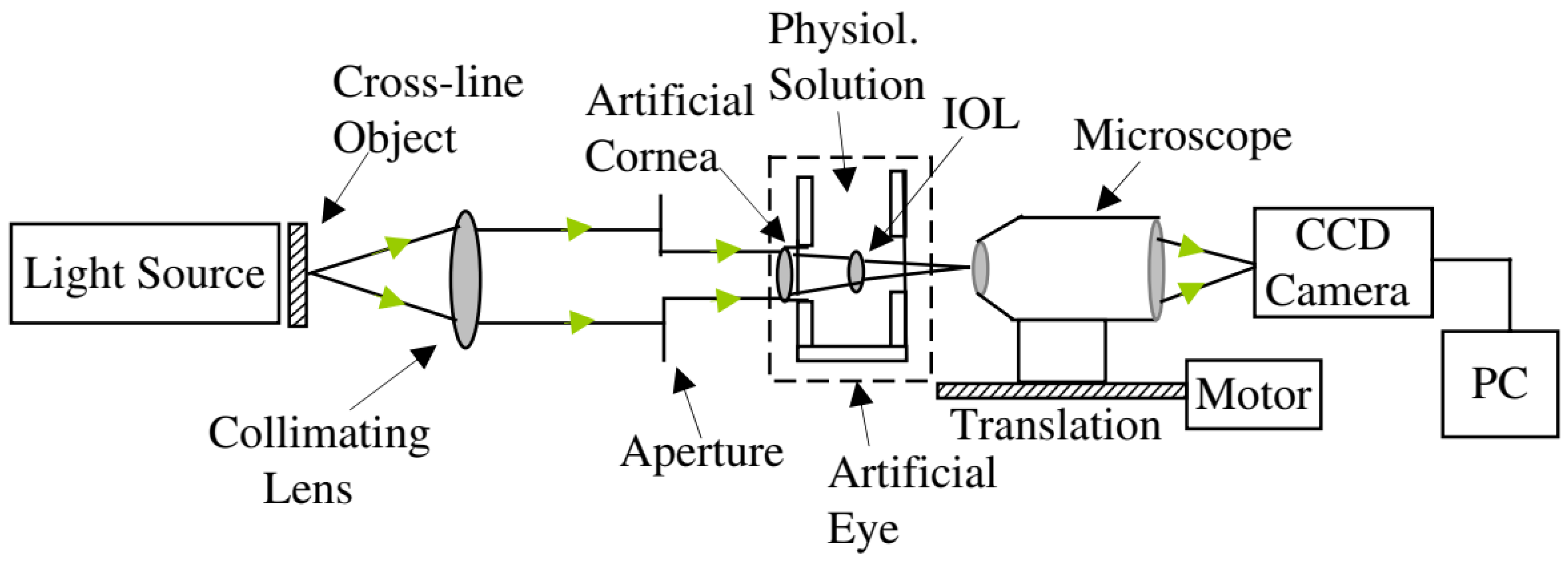
Figure 4.
Schematic diagram of the eye model configuration used by Artigas et al, based on the ISO standards. Journal of Cataract and Refractive Surgery 2007, 33, 2111–2117 ([25]). Originally published by and reprinted with permission from Lippincott Williams & Wilkins, Inc.Norrby et al. [23] created and implemented one of their theoretical models as a physical device for MTF measurements (Figure 5). It seemed very simple and had the interesting characteristic of being packed into a very small enclosure, which could easily fit in different experimental setups. A CCD camera and suitable relay optics would simulate what the patient sees. The authors also mentioned the possibility of modifying it for wavefront measurements by using a diffusing retina, suggesting it could be used both for wavefront and single-pass measurements. Other single-pass models have been presented before as multi-modal cases [23,28]. Additional single-pass models for image formation will be presented in a later section dedicated to human vision.
Figure 4.
Schematic diagram of the eye model configuration used by Artigas et al, based on the ISO standards. Journal of Cataract and Refractive Surgery 2007, 33, 2111–2117 ([25]). Originally published by and reprinted with permission from Lippincott Williams & Wilkins, Inc.Norrby et al. [23] created and implemented one of their theoretical models as a physical device for MTF measurements (Figure 5). It seemed very simple and had the interesting characteristic of being packed into a very small enclosure, which could easily fit in different experimental setups. A CCD camera and suitable relay optics would simulate what the patient sees. The authors also mentioned the possibility of modifying it for wavefront measurements by using a diffusing retina, suggesting it could be used both for wavefront and single-pass measurements. Other single-pass models have been presented before as multi-modal cases [23,28]. Additional single-pass models for image formation will be presented in a later section dedicated to human vision.
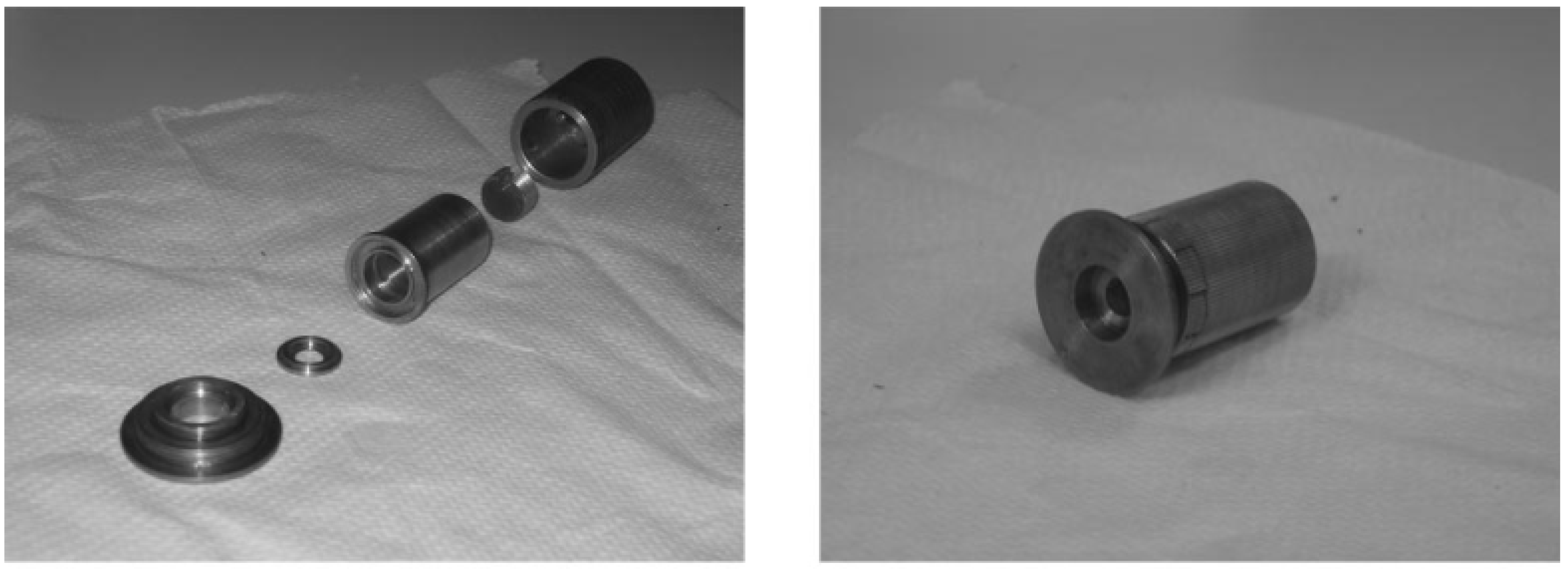
Figure 5.
Photograph of the device used by Norrby et al.: (Left) individual parts; (Right) fully assembled device. An interesting feature of this eye model is the fact it is all its components are compacted into a small enclosure, whose size resembles a real eye. Applied Optics 2007, 46, 6595–6605 ([23]). Originally published by and reprinted with permission from Optica Publishing Group.
Figure 5.
Photograph of the device used by Norrby et al.: (Left) individual parts; (Right) fully assembled device. An interesting feature of this eye model is the fact it is all its components are compacted into a small enclosure, whose size resembles a real eye. Applied Optics 2007, 46, 6595–6605 ([23]). Originally published by and reprinted with permission from Optica Publishing Group.
There are also single-pass techniques that do not involve the formation of a retinal image. Sheehy et al. [76] described in a patent application an artificial human eye, around 6.5 times the size of a natural eye, for testing the effectiveness of protective eyewear against harmful radiation (e.g., laser, ultraviolet rays, etc.). A transparent or translucent image plane functioned as the retina, which could be connected to a CCD, an optometer, a radiometer, etc. Radiation intensity could then be quantified, by analyzing pixel intensity, radiation levels, etc.
Regal et al. [70] developed an optomechanical eye model phantom by combining optical light propagation and thermal characteristics, to provide a system for accurately modeling the effects of laser surgery. This model was mainly composed of a main body and ancillary optical components, and a tunable microfluidic iris, and was fabricated using a 3D printed holder and modified polydimethylsiloxane. It also included a cornea, lens, ciliary body, sclera, and phosphate buffered saline (BSS) emulating aqueous and vitreous humors. A LED light source was mounted in the stand 1 mm in front of the cornea and directed into the iris for optical single-pass measurements. A concave depression in the center of the design simulated the retina at the back of the eye, where a photodiode was located for single-pass optical measurements performed for different angles, to compute the transmissibility of the pupil. Thermal measurements were also performed and will be detailed later in a dedicated sub-section.
Other single-pass techniques involve laser ray-tracing (LRT). Such an example is presented by Moreno-Barriuso et al. [9]. Another case is presented by Barbero et al. [16], where a model with a camera objective as the cornea and a diffuser surface was placed at the focal plane, acting as the retina. Aerial images were captured by a camera for a ray optics analysis. To avoid speckle noise in the aerial images, laser exposure times were increased while the diffuser was moved vertically. Wave aberrations were computed from the images. Eppig et al. [36] used single-pass ray-tracing to assess the effect of decentration and tilt on the image quality of aspheric IOL designs in a model eye. The model was based on the Liou-Brennan model eye [93], and included a pupil decentered nasally by 0.50 mm, resulting in a visual axis, which is tilted by 5 degrees (“kappa”) relative to the optical axis. The model also incorporated slight crystalline lens decentration (approximately 0.50 mm temporally) and tilt (<5 degrees relative to the line of sight), which showed good agreement with previous phakometric measurements. The wet-cell-based model of Terwee et al. [27]